Mvp-paroxetine-v01 .doc
Methode validatie protocol Bepaling van Paroxetine in serum Documentnummer: MVP-Paroxetine Versie: 01 Document samenstelling, review en goedkeuring : Datum en handtekening PDF created with pdfFactory trial version INTRODUCTIE . 3 De te bepalen component(en) . 3 De analytische methode . 4 UITVOERING VAN DE METHODE VALIDATIE . 6 Het methode validatie protocol
 European Heart Journal Advance Access published November 29, 2006
European Heart Journal Advance Access published November 29, 2006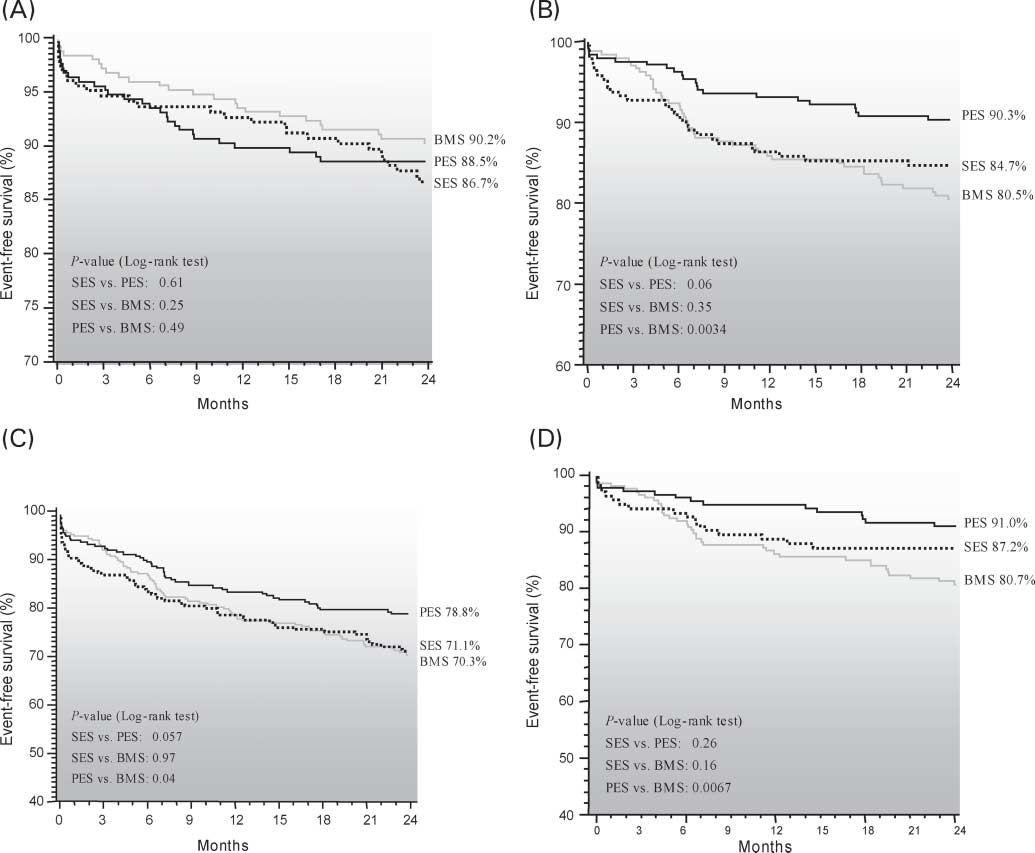 Two-year cumulative incidence of mortality (A), TVR (B), major adverse cardiac events (C), and TVR in NIDDM (D), in patients treated with BMS, SES, or
the BMS patients, vs. 18.2% and 14.7% of the SES and PES
died, seven presented with an MI, and 12 patients were
patients, respectively (P ¼ 0.33 SES vs. PES). TLR was per-
still on dual-antiplatelet therapy at the time of the event.
Two-year cumulative incidence of mortality (A), TVR (B), major adverse cardiac events (C), and TVR in NIDDM (D), in patients treated with BMS, SES, or
the BMS patients, vs. 18.2% and 14.7% of the SES and PES
died, seven presented with an MI, and 12 patients were
patients, respectively (P ¼ 0.33 SES vs. PES). TLR was per-
still on dual-antiplatelet therapy at the time of the event.